Introduction
Schedule I is an audacious late-2025 indie breakout from Tyler’s Video Game Studio (TVGS), thrusting players into the chaotic world of crime-themed tycoon simulation. As a first-person sandbox, it empowers you to transition from a street-level hustler to a drug empire kingpin in the fictional city of Hyland Point. With its dark humor, surprising crafting depth, and cooperative chaos, it quickly became one of the most played and talked-about titles on Steam.
Core Gameplay Loop
- Drug Crafting & Innovation: Start small with marijuana cultivation and expand into more potent substances. Unique fictional recipes—a mix of weed with soda or paracetamol—unlock bizarre effects from visual changes to explosions, enhancing both strategy and absurdity.
- Business Expansion: Hire employees, secure properties, automate production chains, launder money, and scale operations across town—all while buyers, suppliers, and carts of cash spin your growing enterprise forward.
- Open-World Mayhem: Traverse Hyland Point on foot, skateboard, or drive as you evade police, outsmart rival cartels, or engage them with weaponry—all dripping with criminal theatrics.
- Cooperative Multiplayer: Up to four players can divide roles: cultivating, packaging, dealing, and defending, turning the grind into hilarious team-building sessions.
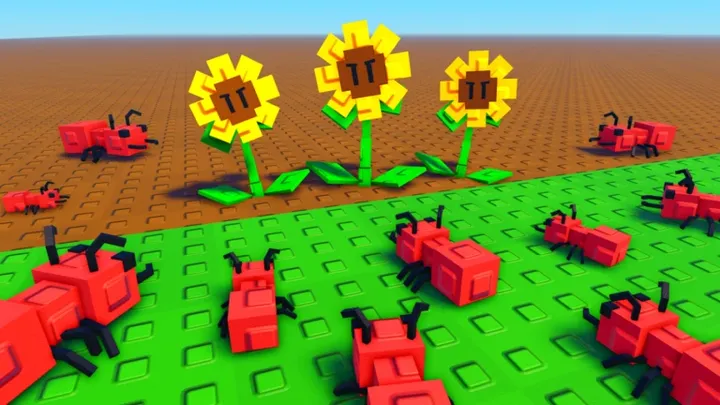
Presentation & Tone
- Stylized & Satirical: The game’s cartoonish, exaggerated visuals clash intentionally with its mature themes, aligning its vibe somewhere between “Breaking Bad” and “Rick & Morty parody.”
- Dark Comedy: Wry dialogue, over-the-top crafting recipes, and pun-heavy badges lend a comedic edge to what could otherwise be grim gameplay.
- Accessible Depth: The intuitive but layered interface makes building and managing a criminal empire feel fun rather than overwhelming.
Strengths
- VAULT of Viral Appeal: Its unusual mechanics and humor made it a hit among streamers and TikTok communities, propelling high player numbers and solid review ratings.
- Engaging Mini-Games: Every step—from mixing to selling—is a quick, interactive sequence that keeps the gameplay loop lively.
- Flexible Progression: Whether you want a solo spree or chaotic co-op run, the game adapts, with automation allowing later-stage idle income.
- Surprisingly Deep Management: Despite its indie roots, the systems for supply chains, territory control, and automation feel robust and satisfying.
- Rapid Iteration: Even in early access, the developer releases frequent content updates and engages directly with player feedback.
Weaknesses
- Repetitive Late Game: Once your drug empire is automated, the gameplay can lose momentum and feel grindy.
- Solo Runs Lag: Playing alone can struggle with pacing, as some systems work best when automated or handled by friends.
- Performance Issues After Long Sessions: Reports of crashes or glitches appear after dense, extended gameplay.
- Ethical Gray Area: While stylized, the theme may be jarring for those sensitive to realistic depictions of illicit activities.
- Legal Overlap: Comparisons to other drug-dealer-themed games have sparked debate, though no litigation has followed yet.
Community Dynamics
Discussions across forums emphasize how Schedule I is more than a simulator—it’s a co-op playground where players strategize, joke, and improvise. Even the wildest crafting combos and heists become memorable group stories. However, many also note that solo play feels shallow without a social component. Some fans request more variety in world events or consequences to keep post-campaign gameplay fresh.
Final Verdict
Schedule I reinvents tycoon simulation with boldness, humor, and slick gameplay loops. Its success shows the power of indie creativity on a global stage. While it stumbles in later phases and may not suit all tastes, its fresh take and co-op charm make it far more than a passing meme—it’s a standout in modern indie design.